Development Through the Lifespan 6th Edition Chapter 11
11 Chapter 11: Late Adulthood


Photos Courtesy of Pixabay (left) and Rosanetur (right)
Objectives:
At the end of this lesson, you will be able to…
- Differentiate between impaired, normal, and optimal aging.
- Report numbers of people in late adulthood age categories in the United States.
- Discuss changes in the age structure of society in the U. S. and globally.
- Report life expectancies in the United States based on gender, race, and ethnicity.
- Explain the reasons for changes in life expectancies.
- Identify examples of ageism.
- Compare primary and secondary aging.
- Report on the leading sources of secondary aging.
- Describe changes in the senses in late adulthood.
- Discuss the impact of aging on the sensory register, working memory, and long-term memory.
- Describe theories of aging.
- Define Hayflick Limit.
- Evaluate previous ideas about aging and cognition based on new research.
- Describe abnormal memory loss due to Alzheimer's disease, delirium, and dementia.
- Differentiate between organic and nonorganic causes of dementia.
- Describe Erikson's psychosocial stage for late adulthood.
- Contrast disengagement, activity, and continuity theories of aging.
- Describe ways in which people are productive in late adulthood.
- Describe grandparenting styles.
- Compare marriage, divorce, being single, and widowhood in late adulthood.
- Report rates at which people in late adulthood require long-term care.
- Examine caregiving for dependent older adults.
- Define socioemotional selectivity theory.
- Classify types of elder abuse.
The objectives are indicated in the reading sections below.
Introduction
We are considered to be in late adulthood from the time we reach our mid-sixties until death. For the purpose of this textbook and chapter, we will define late adulthood from age 65 to 100 and beyond. This is the longest developmental stage across the lifespan. In this chapter, we will learn how many people are in late adulthood, how that number is expected to change, and how life changes and continues to be the same as before in late adulthood. We will also examine several theories of human aging, the physical, cognitive, and socioemotional changes that occur with this population, and the vast diversity among those in this developmental stage.
Physical Development in Late Adulthood
Defining Late Adulthood: Age or Quality of Life? (Ob 1)
About 14.9 percent of the U. S. population or 47.8 million Americans are 65 and older (U. S. Census Bureau, 2015). This number is expected to grow to 98.2 million by the year 2060 at which time people over 65 will make up 25 percent of the population. Currently, one in seven Americans is 65 years of age or older, and by the year 2050, almost one in four Americans will be over 65. This group varies considerably and is divided into categories of 65 plus, 85 plus, and centenarians for comparison by the census. Of this number, 19.7 million will be age 85 or older. Developmentalists, however, divide this population into categories based on health and social well-being. Optimal aging refers to those who enjoy better health and social well-being than average. Normal aging refers to those who seem to have the same health and social concerns as most of those in the population. However, there is still much being done to understand exactly what normal aging means. Impaired aging refers to those who experience poor health and dependence to a greater extent than would be considered normal. Aging successfully involves adjusting as needed in order to continue living as independently and actively as possible. This is referred to as selective optimization with compensation and means, for example, that a person who can no longer drive, is able to find alternative transportation. Or a person who is compensating for having less energy learns how to reorganize the daily routine to avoid overexertion. Perhaps nurses and other allied health professionals working with this population will begin to focus more on helping patients remain independent than on simply treating illnesses. Promoting health and independence are important for successful aging.
Age Categories (Ob 2)
There have been many ways to categorize the ages of individuals in late adulthood. In this chapter, we will be dividing the stage into age categories. These categories are based on the conceptions of aging including, biological, psychological, social, and chronological differences. They also reflect the increase in longevity of those living to this latter stage.
65 to 74: These 18.3 million Americans tend to report greater health and social well-being than older adults. Having good or excellent health is reported by 41% of this age group (Center for Disease Control, 2004). Their lives are more similar to those of midlife adults than those who are 85 and older. This group is less likely to require long-term care, to be dependent or to be poor, and more likely to be married, working for pleasure rather than income, and living independently. About 65% of men and 50% of women between the ages of 65-69 continue to work full-time (He, Sengupta, Velkoff, & DeBarros, 2005). Physical activity tends to decrease with age, despite the dramatic health benefits enjoyed by those who exercise. People with more education and income are more likely to continue being physically active. And males are more likely to engage in physical activity than are females. The majority of the young-old continue to live independently. Only about 3% of those 65-74 need help with daily living skills (compared with about 22.9% of people over 85). (Another way to consider think of this is that 97% of people between 65-74 and 77% of people over 85 do not require assistance!) This age group is less likely to experience heart disease, cancer, or stroke than the old, but nearly as likely to experience depression (U. S. Census, 2005).
75 to 84: This age group is more likely to experience limitations on physical activity due to chronic diseases such as arthritis, heart conditions, hypertension (especially for women), and hearing or visual impairments. Rates of death due to heart disease, cancer, and cerebral vascular disease are double that experienced by people 65-74. Compared to those over 85, this group is less likely to require long-term care, to be dependent or poor, and more likely to be married, working for pleasure rather than income, and living independently. The majority of these 12.9 million Americans live independently or with relatives. Overall, those in this age period feel a sense of happiness and emotional well-being that is better than at any other period of adulthood (Carstensen, Fung, & Charles, 2003; George, 2009; Robins & Trzesniewski, 2005). Widowhood is more common in this group-especially among women. In 2018, 39% of women ages 75 to 84 lived alone (U.S. Census, 2018). Poverty rates are 3 percent higher (12 percent) than for those between 65 and 74.
Young-Old (65-84) recap: Older adults between the ages of 65 and 84 comprise the "young-old" (Ortman et al., 2014). The young-old experience relatively good health and social engagement (Smith, 2000), knowledge and expertise (Singer, Verhaeghen, Ghisletta, Lindenberger, & Baltes, 2003), and adaptive flexibility in daily living (Riediger, Freund, & Baltes, 2005). The young-old also show strong performance in attention, memory, and crystallized intelligence. In fact, those identified as young-old are more similar to those in midlife than those who are 85 and older. This group is less likely to require long-term care, to be dependent or poor, and more likely to be married, working for pleasure rather than income, and living independently. Chronic diseases, such as cardiovascular disease, hypertension, and cancer, are among the most common (especially later in this period), but because they are linked to lifestyle choices, they typically can be can prevented, lessoned, or managed (Barnes, 2011b).
Oldest-old: The "oldest-old" are those 85 and over. The number of people 85 and older is 34 times greater than in 1900 and now includes 5.7 million Americans. This age group is one of the fastest growing worldwide. The oldest-old are projected to be nearly 18 million by 2050, showing an increase more than 300% over its current levels (NIA, 2015b). Females comprise more than 60% of those 85 and older, but they also suffer from more chronic illnesses and disabilities than older males (Gatz et al., 2016). While this age group currently accounts for 2% of the U. S. population, it accounts for 9% of all hospitalizations (Levant, Chari & DeFrances, 2015). Those 85 and up are less likely to be discharged and more likely to die in hospital. The most common reasons for hospitalization for the oldest-old were congestive heart failure, pneumonia, urinary tract infections, septicemia, stroke, and hip fractures. In recent years, hospitalizations for many of these medical problems have been reduced. However, hospitalization for urinary tract infections and septicemia has increased for those 85 and older.
This group is more likely to require long-term care and to be in nursing homes. The oldest-old are less likely to be married and living with a spouse compared with the majority of the young-old (APA, 2016; Stepler, 2016c). Almost 50% of the oldest-old require some assistance with daily living activities (APA, 2016). However, of the 38.9 million American over 65, only 1.6 million require nursing home care. Sixty-eight percent live with relatives and 27 percent live alone (He et al., 2005; U. S. Census Bureau, 2011). In 2018, 55% of women ages 85 and older lived alone (U.S. Census Bureau, 2018).
Centenarians: A segment of the oldest-old are centenarians, that is, 100 and older (Wilcox, Wilcox & Ferrucci, 2008). In 2015 there were nearly half a million centenarians worldwide, and it is estimated that this age group will grow to almost 3.7 million by 2050. The U. S. has the most centenarians, but Japan and Italy have the most per capita (Stepler, 2016e). Most centenarians tended to be healthier than many of their peers as they were growing older, and often there was a delay in the onset of any serious disease or disability until their 90s. 53,364 is the number of people age 100 and older counted by the 2010 US Census. In 2010, over half (62.5 percent) of the 53,364 centenarians were age 100 or 101. The ratio of men to women centenarian is 1:5 (20 men for every 100 women). Additionally, 25% reached 100 with no serious chronic illnesses, such as depression, osteoporosis, heart disease, respiratory illness, or dementia (Ash et al. 2015).
The "Graying" of America and the globe (Ob 3)
According to the U. S. Census Bureau (2014b) a person who turned 65 in 2015 can expect to live another 19 years, which is 5.5 years longer than someone who turned 65 in 1950. This increasingly aged population has been referred to as the "Graying of America." This "graying" is already having significant effects on the nation in many areas, including work, health care, housing, social security, caregiving, and adaptive technologies. Interestingly, populations are aging in most other countries of the world. One exception to this is in sub-Saharan Africa where mortality rates are high due to HIV/AIDS (He et al., 2005). There are 520 million people over 65 worldwide (8 percent) and that number is expected to increase to 17 percent by 2050. Currently, four countries, Germany, Italy, Japan, and Monaco have 20 percent of their population over 65. China has the highest number of people over 65 at 112 million (U. S. Census Bureau, 2011), while Japan has the highest percentage of individuals 65 and older. In total number, the United States is projected to have a larger older population than the other developed nations, but a smaller older population compared with China and India, the world's two most populous nations (Ortman et al., 2014). Between 2012 and 2050, the proportion aged 65 and over is projected to increase in all developed countries. By 2050, China's older population is projected to grow larger than the total U.S. population today.
As the population ages, concerns grow about who will provide for those requiring long-term care. In 2000, there were about 10 people 85 and older for every 100 persons between ages 50 and 64. These midlife adults are the most likely care providers for their aging parents. The number of old requiring support from their children is expected to more than double by the year 2040 (He et al., 2005). These families will certainly need external physical, emotional, and financial support in meeting this challenge. Further the aging of the baby boom generation (1944-1964) could fuel more than a 50 percent increase in the number of Americans ages 65 and older requiringnursing home care, to about 1.9 million in 2030 from 1.2 million in 2017 (Population Reference Bureau, 2019).
Life Expectancy and Quality of Life (Ob 4, Ob 5)
Lifespan or Maximum Lifespan is referred to as the greatest age reached by any member of a given population (or species). For humans, the lifespan is currently between 120 and 125 . Life Expectancy is defined as the average number of years that members of a population (or species) live. According to the World Health Organization (WHO) (2016) global life expectancy at birth in 2015 was 71.4 years. Overall life expectancy ranged from 60.0 years in the WHO African Region to 76.8 years in the WHO European Region. Global life expectancy increased by 5 years between 2000 and 2015, and the largest increase was in the WHO African Region where life expectancy increased by 9.4 years. This was due primarily to improvements in child survival and access to antiretroviral medication for the treatment of HIV. According to the Central Intelligence Agency (2016) the United States ranks 43rd in the world for life expectancy.
Globally we see a gender gap, with a life expectancy rate of 73.8 years for females and males reaching 69.1 years (WHO, 2016). Although globally, women live longer than men around the world although the female advantage differs country to country. For example, in Russia women live 10 years longer than men, but in Bhutan (South Asia) the differenc is less than 6 months. In the United States, the gap between the sexes has existed for over 120 years. It was seven years since 1990, but in 2017, this gap had narrowed to five years (76.1 years versus 81.1 years) (Murphy, 2018).
Table. US Life expectancy rates
| Year | Females | Males | Gender gap |
| 1900 | 48.3 | 46.3 | 2 years |
| 1950 | 71.1 | 65.6 | 5.5 years |
| 1990 | 78.8 | 71.8 | 7 years |
| 2000 | 79.7 | 74.3 | 5.4 years |
| 2017 | 81.1 | 76.1 | 5 years |
Source: National Center for Health Statistics
Within the U.S., there are also differences in life expectancy when examining racial groups. … Historic racism or years of living under oppressive prejudice and discrimination can increase the incidence of stress-related illness and contribute to a lower life expectancy. Wide economic disparities are evident across different population subgroups. Among adults ages 65 and older, 17 percent of Latinos and 19 percent of African Americans lived in poverty in 2017—more than twice the rate among older non-Hispanic whites (7 percent) (U.S. Census Bureau, Annual Social and Economic Supplement, 2017). The older population is becoming more racially and ethnically diverse . Between 2018 and 2060 the share of the older population that is non-Hispanic white is projected to drop from 77 percent to 55 percent (U.S. Census Bureau, Population Projections, 2017).Despite the increased diversity in the older adult population, the more rapidly changing racial/ethnic composition of the population under age 18 relative to those ages 65 and older has created a diversity gap between generations.
Table. US Life expectancy rates across sexes
| Year | All races | African American 1 | White 1 |
| 1900 | 47.3 | 33 | 47.6 |
| 1950 | 68.2 | 60.8 | 69.1 |
| 1990 | 75.4 | 69.1 | 76.1 |
| 2000 | 76.8 | 71.8 | 77.3 |
| 2015 | 78.7 | 75.5 | 78.9 |
Source: National Center for Health Statistics,
1Non-Hispanic
Increased life expectancy brings concern over the health and independence of those living longer. When looking at large populations, the WHO (2016) measures how many equivalent years of full health on average a newborn baby is expected to have. This age considers current age-specific mortality, morbidity, and disability risks and is referred to as the Healthy Life Expectancy (HLE). In 2015, the global Healthy Life Expectancy was 63.1 years up from 58.5 years in 2000. The WHO African Region had the lowest Healthy Life Expectancy at 52.3 years, while the WHO Western Pacific Region had the highest at 68.7 years. In the United States, the overall life expectancy is 79.7 years, however, life expectancies vary by sex, race, and ethnicity. The highest Healthy Life Expectancy (HLE) was observed in Hawaii with 16.2 years of additional good health, and the lowest was in Mississippi with only 10.8 years of additional good health. Overall, the lowest HLE was among southern states.In the United States, females had a greater HLE than males at age 65 years in every state and DC. HLE was greater for whites than for blacks in DC and all states from which data were available, except in Nevada and New Mexico.
The shorter life expectancy for men, in general, is attributed to greater stress, poorer attention to health, more involvement in dangerous occupations, and higher rates of death due to accidents, homicide, and suicide. Men are more likely to contract viral and bacterial infections, and their immunity at the cellular level decreases significantly faster with age. Although women are slightly more prone to autoimmune and inflammatory diseases, such as rheumatoid arthritis, the gradual deterioration of the immune system is slower in women (Caruso, Accardi, Virruso, & Candore, 2013; Hirokawa et al., 2013). Additionally, men are less likely than women to have health insurance, develop a regular relationship with a doctor, or seek treatment for a medical condition (Scott, 2015). Lastly, social contact is also important as loneliness is considered a health hazard. Nearly 20% of men over 50 have contact with their friends less than once a month, compared to only 12% of women who see friends that infrequently (Scott, 2015). Social support can increase longevity. For men, life expectancy and health seem to improve with marriage. Spouses are less likely to engage in risky health practices and wives are more likely to monitor their husband's diet and health regimes. But men who live in stressful marriages can also experience poorer health as a result.

Photo Courtesy of Jordan Fisher
Key players in improving the quality of life among older adults will be those adults. By exercising, reducing stress, stopping smoking, limiting the use of alcohol, and consuming more fruits and vegetables, older adults can expect to live longer and more active lives (He et al, 2005). Stress reduction both in late adulthood and earlier in life is also crucial. The reduction of societal stressors can promote active life expectancy. In the last 40 years, smoking rates have decreased, but obesity has increased, and physical activity has only modestly increased.
Here are 13 tips to get you on your way to aging well (adapted from APA (1998), John Hopkins (2020), and Harvard Health (2019):
1. Don't smoke. Avoid tobacco in all its forms.
2. Make healthy food choices. That means eating more healthful foods and fewer harmful foods.
- Eat more: whole grains, fruits, vegetables and legumes, fish, low- or non-fat dairy products, and nuts and seeds.
- Eat less: red meat, whole-milk dairy products, poultry skin, high-sodium (salty) processed foods, sweets, sugary drinks and refined carbohydrates, and if you need to lose weight, calories.
3. Exercise regularly, including:
- At least 30 minutes of moderate exercise nearly every day.
- Exercises for strength two to three times a week.
- Exercises for flexibility and balance according to need.
- A moderate amount each day can help one stay active, independent, and maintain positive mood.
4. Loose weight and keep it off. Stay lean. It's equally hard for men and women, but even partial success will help. Successful weightloss depends on being aware of your behaviors and making changes to them.
5. Limit alchol intake. If you choose to drink, limit yourself to one to two drinks a day, counting 5 ounces of wine, 12 ounces of beer, and 1.5 ounces of liquor as one drink.
6. Reduce stress. Get enough sleep. Build social ties and community support.
7. Avoid risky behavior, including drug abuse, unsafe sex, dangerous driving, unsafe firearm use, and living in hazardous household conditions.
8. Reduce exposure to toxins and radiation, including sunlight and medical x-rays.
9. Get regular medical check-ups, screening tests, and immunizations. Listen to your body and report sounds of discord to your doctor.
- Engage in routine preventive health behaviors (e.g., check ups and immunizations).
- Be your advocate in health care settings (or bring a knowledgeable person with you). Do not be afraid to ask questions or seek a second opinion.
10. Maintain a healthy lifestyle and make adjustments for any changes that may happen as you age (e.g., vision, strength).
11. If you feel anxious, depressed, or are using alcohol or drugs to manage your mood, seek assistance. Untreated mental health problems are associated with a decreased quality of life, and poor physical health outcomes (e.g., increased disability and illness).
12. Be an interested and interesting person. Remain aware of new developments in the arts, sciences, politics, and other areas of cultural and social interest. Engage in something that matters to you and that you care passionately about.
13. Seek joy and share it with others. Laughter is good medicine. Fun and optimism improve health as well as happiness.
Attitudes about Aging (Ob 6)
Stereotypes about people in late adulthood lead many to assume that aging automatically brings poor health and mental decline. These stereotypes are reflected in everyday conversations, the media and even in greeting cards (Overstreet, 2006). The following examples serve to illustrate stereotypes about old age.
- Grandpa, fishing pole in one hand, pipe in the other, sits on the ground and completes a story being told to his grandson with ". . . and that, Jimmy, is the tale of my very first colonoscopy." The message inside the card reads, "Welcome to the gross personal story years." (Shoebox, A Division of Hallmark Cards.)
- An older woman in a barber shop cuts the hair of an older, dozing man. "So, what do you say today, Earl?" she asks. The inside message reads, "Welcome to the age where pretty much anyplace is a good place for a nap." (Shoebox, A Division of Hallmark Cards.)
- A crotchety old man with wire glasses, a crumpled hat, and a bow tie grimaces and the card reads, "Another year older? You're at the age where you should start eatin' right, exercisin', and takin' vitamins . . ." The inside reads, "Of course you're also at the age where you can ignore advice by acting like you can't hear it." (Hallmark Cards, Inc.)
Of course, these cards are made because they are popular. Age is not revered in the United States, and so laughing about getting older is one way to get relief. The attitudes are examples of ageism, prejudice based on age. Stereotypes such as these can lead to a self-fulfilling prophecy in which beliefs about one's ability results in actions that make it come true. For older adults, their perceptions of aging—and their self-perceptions—can have serious effects on their health, behaviors, and even longevity. A positive, optimistic outlook about aging and the impact one can have on improving health is essential to health and longevity. A negative view about one's physical abilities as associated with physical losses might impair health-related strategies that are important for maintaining a healthy lifestyle (Wurm, Warner, Ziegelmann, Wolf, & Schüz, 2013). Removing societal stereotypes about aging and helping older adults reject those notions of aging is another way to promote health and active life expectancy among the old.

Photo Courtesy of Patrick
Primary and Secondary Aging (Ob 7, Ob 9)
Healthcare providers need to be aware of which aspects of aging are reversible and which ones are inevitable. By keeping this distinction in mind, caregivers may be more objective and accurate when diagnosing and treating older patients. And a positive attitude can go a long way toward motivating patients to stick with a health regime. Unfortunately, stereotypes can lead to misdiagnosis. For example, it is estimated that about 10 percent of older patients diagnosed with dementia are actually depressed or suffering from some other psychological illness (Berger, 2005). The failure to recognize and treat psychological problems in older patients may be one consequence of such stereotypes.
The Baltimore Longitudinal Study on Aging (BLSA) (NIA, 2011b) began in 1958 and has traced the aging process in 1,400 people from age 20 to 90. Researchers from the BLSA have found that the aging process varies significantly from individual to individual and from one organ system to another. However, some key generalization can be made including heart muscles thickening with age, arteries become less flexible, and lung capacity diminishing. Kidneys become less efficient in removing waste from the blood, and the bladder loses its ability to store urine. Brain cells also lose some functioning, but new neurons can also be produced. Many of these changes are determined by genetics, lifestyle, and disease. However, some generalizations about the aging process have been found:
- Heart muscles thicken with age
- Arteries become less flexible
- Lung capacity diminishes
- Brain cells lose some functioning but new neurons can also be produced
- Kidneys become less efficient in removing waste from the blood
- The bladder loses its ability to store urine
- Body fat stabilizes and then declines
- Muscle mass is lost without exercise
- Bone mineral is lost. Weight-bearing exercise slows this down.
Let's examine the aging process a bit more identifying primary and secondary aging processes. Primary aging refers to the inevitable changes associated with aging (Busse, 1969). These changes include changes in the skin and hair, height and weight, hearing loss, and eye disease. However, some of these changes can be reduced by limiting exposure to the sun, eating a nutritious diet, and exercising.

Photo Courtesy of Florida Memory
Skin and hair change as we age. The skin becomes drier, thinner, and less elastic as we age. Gravity can cause the skin to sag and wrinkle, and smoking can wrinkle the skin. Scars and imperfections become more noticeable as fewer cells grow underneath the surface of the skin. Exposure to the sun, or photoaging, accelerates these changes. Older people may bruise more easily, and it can take longer for these bruises to heal. Some medicines or illnesses may also cause bruising. Also, seen in older adults are age spots, previously called "liver spots." They look like flat, brown spots and are often caused by years in the sun. Skin tags are small, usually flesh-colored growths of skin that have a raised surface. They become common as people age, especially for women, but both age spots and skin tags are harmless (NIA, 2015f). Nearly everyone has hair loss as they age, and the rate of hair growth slows down as many hair follicles stop producing new hairs. The loss of pigment and subsequent graying begun in middle adulthood continues in late adulthood. Graying hair is inevitable.
Height and weight vary with age. Older people are more than an inch shorter than they were during early adulthood (Masoro in Berger, 2005). The tendency to become shorter as one ages occurs among all races and both sexes. Height loss is related to aging changes in the bones, muscles, and joints. Height loss is due to a settling of the vertebrae and a lack of muscle strength in the back. Bones lose density and may become brittle. People typically lose almost one-half inch every 10 years after age 40, and height loss is even more rapid after age 70. A total of 1 to 3 inches in height is lost with aging. Weight training can help increase bone density after just a few weeks of training.
Muscle loss occurs in late adulthood and is most noticeable in men as they lose muscle mass. Maintaining strong leg and heart muscles are important for independence. As discussed in chapter 10, sarcopenia is the loss of muscle tissue as a natural part of aging. Symptoms include a loss of stamina and weakness, which can decrease physical activity and subsequently further shrink muscles. Any loss of muscle is important because it lessens strength and mobility, and sarcopenia is a factor in frailty and the likelihood of falls and fractures in older adults. Maintaining strong leg and heart muscles are important for independence. Weight-lifting, walking, swimming, or engaging in other cardiovascular exercises can help strengthen the muscles and prevent atrophy.
Figure caption: Top-left normal vision; top-right: cataract; bottom-left: macular degeneration; bottom-right: glaucoma. Photo Courtesy of WikiCommons
Visual Problems: The majority of people over 65 have some difficulty with vision, but most are easily corrected with prescription lenses. Three percent of those 65 to 74 and 8 percent of those 75 and older have hearing or vision limitations that hinder activity. The most common causes of vision loss or impairment are glaucoma, cataracts, and age-related macular degeneration (He et al., 2005). Cataracts are a clouding of the lens of the eye. The lens of the eye is made up of mostly water and protein. The protein is precisely arranged to keep the lens clear, but with age, some of the protein starts to clump. As more of the protein clumps together the clarity of the lens is reduced. While some adults in middle adulthood may show signs of cloudiness in the lens, the area affected is usually small enough to not interfere with vision. By age 75, 70% of adults will have problems with cataracts (Boyd, 2014). Cataracts also cause a discoloration of the lens, tinting it more yellow and then brown, which can interfere with the ability to distinguish colors such as black, brown, dark blue, or dark purple. Older adults are also more likely to develop age-related macular degeneration, which is the loss of clarity in the center field of vision, due to the deterioration of the macula, the center of the retina. Macular degeneration does not usually cause total vision loss, but the loss of the central field of vision can greatly impair day-to-day functioning. A third vision problem that increases with age is glaucoma, which is the loss of peripheral vision, frequently due to a buildup of fluid in the eye that damages the optic nerve. As you age the pressure in the eye may increase causing damage to the optic nerve. The exterior of the optic nerve receives input from retinal cells on the periphery, and as glaucoma progresses more and more of the peripheral visual field deteriorates toward the central field of vision. In the advanced stages of glaucoma, a person can lose their sight. Fortunately, glaucoma tends to progress slowly (NEI, 2016b). There is no cure for glaucoma, but its rate of progression can be slowed, especially with early diagnosis. Routine eye exams to measure eye pressure and examination of the optic nerve can detect both the risk and presence of glaucoma (NEI, 2016b). Those with elevated eye pressure are given medicated eye drops. Reducing eye pressure lowers the risk of developing glaucoma or slow its progression in those who already have it.
Hearing Loss is experienced by 30 percent of people age 70 and older. Almost half of the people over 85 have some hearing loss (He et al., 2005). Among those who are in nursing homes, rates are higher. Presbycusis is a common form of hearing loss in late adulthood that results in a gradual loss of hearing. It runs in families and affects hearing in both ears (NIA, 2015c). Older adults may also notice tinnitus, a ringing, hissing, or roaring sound in the ears. The exact cause of tinnitus is unknown, although it can be related to hypertension and allergies. It may come and go or persist and get worse over time (NIA, 2015c). The incidence of both presbycusis and tinnitus increase with age and males have higher rates of both around the world (McCormak, Edmondson-Jones, Somerset, & Hall, 2016). Smoking, middle ear infections, and exposure to loud noises increase hearing loss.
| Common Signs of Hearing Loss |
|
Older adults are more likely to seek help with vision impairment than with hearing loss, perhaps due to the stereotype that older people who have difficulty hearing are also less mentally alert. Being unable to hear causes people to withdraw from conversation and others to ignore them or shout. Unfortunately, shouting is usually high pitched and can be harder to hear than lower tones. The speaker may also begin to use a patronizing form of 'baby talk' known as elderspeak (See et al., 1999). This language reflects the stereotypes of older adults as being dependent, demented, and childlike. Image others are speaking to you in that way. How would you feel? I am reminded of a man dying at home and a hospice worker, on shift for the first time, comes to his bedside and shouts, "Hi, baby. Want me to rub your little feet?" His response was an indignant look of disapproval.
Your auditory system has two jobs: To help you to hear, and to help you maintain balance. Your balance is controlled by the brain receiving information from the shifting of hair cells in the inner ear about the position and orientation of the body. With age this function of the inner ear declines which can lead to problems with balance when sitting, standing, or moving (Martin, 2014).
Taste and Smell: Our sense of taste and smell are part of our chemical sensing system. Our sense of taste, or gustation, appears to age well. Normal taste occurs when molecules that are released by chewing food stimulate taste buds along the tongue, the roof of the mouth, and in the lining of the throat. These cells send messages to the brain, where specific tastes are identified. After age 50 we start to lose some of these sensory cells. Most people do not notice any changes in taste until ones 60s (NIH: Senior Health, 2016b). Given that the loss of taste buds is very gradual, even in late adulthood, many people are often surprised that their loss of taste is most likely the result of a loss of smell.
Our sense of smell, or olfaction, decreases more with age, and problems with the sense of smell are more common in men than in women. Olfactory cells are located in a small area high in the nasal cavity. These cells are stimulated by two pathways; when we inhale through the nose, or via the connection between the nose and the throat when we chew and digest food. It is a problem with this second pathway that explains why some foods such as chocolate or coffee seem tasteless when we have a head cold. Problems with our chemical senses can be linked to other serious medical conditions such as Parkinson's, Alzheimer's, or multiple sclerosis (NIH: Senior Health, 2016a). Any sudden change should be checked out. Loss of smell can change a person's diet, with either a loss of enjoyment of food and eating too little for balanced nutrition or adding sugar and salt to foods that are becoming blander to the palette.
Touch: Research has found that with age, people may experience reduced or changed sensations of vibration, cold, heat, pressure, or pain (Martin, 2014). Many of these changes are also aligned with a number of medical conditions that are more common among the elderly, such as diabetes. However, there are changes in the touch sensations among healthy older adults. The ability to detect changes in pressure have been shown to decline with age, with it being more pronounced by the 6th decade and diminishing further with advanced age (Bowden & McNelty, 2013). Yet, there is considerable variability, with almost 40% showing sensitivity that is comparable to younger adults (Thornbury & Mistretta, 1981). Those who show increasing insensitivity to pressure, temperature, or pain are at risk for injury (Martin, 2014).
In summary, primary aging can be compensated for through exercise, corrective lenses, nutrition, and hearing aids. And, more importantly, by reducing stereotypes about aging, people of age can maintain self-respect, recognize their own strengths, and count on receiving the respect and social inclusion they deserve.
Secondary Aging (Ob 8)
Secondary aging refers to changes that are caused by illness or disease. These illnesses reduce independence, impact the quality of life, affect family members and other caregivers, and bring financial burden. Some of the most prevalent illnesses that cause impairment are discussed below. Many issues of secondary aging are chronic illnesses. Chronic illnesses are illnesses that are ongoing, generally incurable conditions that require continuous medical attention and affect daily life. As individuals live longer, diseases that affect older individuals will become more prevalent, and the burden of chronic illness grows with age. Less than 50% of adults 50-64 have a chronic condition, yet 90% aged 75 and up do (Cohen, 2011). Older women are more likely to have a chronic condition than are older men (83% vs. 88%) (CDC, 2009). Other studies place the figure of diabetes in older adults at 26% (CDC, 2014).
Arthritis and other rheumatic conditions are the most common cause of disability among US adults and have been the most common cause of disability among US adults for the past 15 years (NIH: National Institute of Arthritis and Musculoskeletal and Skin Diseases, 2014). Arthritis results in swelling of the joints and connective tissue that limits mobility. According to the NIH, approximately 62% of adults with arthritis are 65 years old and up. Almost 1 in 2 older adults with arthritis have some degree of mobility limitations, such as climbing stairs, walking, and grasping objects. The pain and other limitations of arthritis can also increase the risk of depression and other forms of mental distress. Osteoarthritis is the most common type of arthritis. "When the cartilage, the slick, cushioning surface on the ends of bones wears away, bone rubs against bone, causing pain, swelling, and stiffness. Over time, joints can lose strength and pain may become chronic" (Arthritis Foundation, 2017, para 3). Arthritis is more common among women than men and increases with age. About 19.3 percent of people over 75 are disabled with arthritis; 11.4 percent of people between 65 and 74 experience this disability.
Osteoporosis is a disease that thins and weakens bones to the point that they become fragile and break easily. After age 50, 1 in 2 women and 1 in 4 men will experience an osteoporosis-related fracture in their lifetime, often leading to hip, spine, and wrist fractures (Dailey & Cravedi, 2006). Broken hips are a very serious problem as we age. They greatly increase the risk of death, especially during the year after they break (NIH Senior Health, 2015). In the U.S., more than 53 million adults either already have osteoporosis or at high risk due to low bone mass (NIH Senior Health, 2015). As bones weaken in the spine, adults gradually lose height and their posture becomes hunched over, which is called Kyphosis. Over time a bent spine can make it hard to walk or even sit up. Adults can prevent the loss of bone mass by eating a healthy diet with enough calcium and vitamin D, regularly exercising, limiting alcohol, and not smoking (National Osteoporosis Foundation, 2016). Bone loss is four times more likely in women than in men and becomes even more prevalent in women 85 and older. Whites suffer osteoporosis more than do non-Hispanic Blacks.

Photo Courtesy of Darren Hodson
As discussed in chapter 10, individuals in late adulthood may also experience hypertension, heart disease, stroke, cancer, and diabetes. Hypertension disables 11.1 percent of 65 to 74-year-olds and 17.1 percent of people over 75. Rates are higher among women and Blacks. Rates are highest for women over 75. As discussed in chapter 10, cancer and cardiovascular disease are the overall leading causes of death, and they are especially high reasons for death in middle and late adults. There are changes to the heart that happen with age, and some may increase a person's risk of heart disease. These include stiffening blood vessels and valves, which may result in leaks or problems pumping blood out of the heart (NIA, 2012). There are different types of heart disease, with the most common is atherosclerosis (discussed in chapter 10), the buildup of fatty deposits or plaques in the walls of arteries. As plaque builds up, blood is unable to flow normally and bring oxygen throughout the body, including to the heart. Depending on where the buildup is, atherosclerosis can cause a heart attack, leg pain, or a stroke. Again, atherosclerosis is not part of normal aging. Many of the problems older people have with their heart and blood vessels are caused by disease and not by aging. For example, an older heart can normally pump blood as strong as a younger heart, while less ability to pump blood is caused by disease. Therefore, leading a heart-healthy lifestyle is most important to keeping one's heart strong in late adulthood.
Advancing age is a significant risk factor for cancer, with persons over 65 accounting for 60% of newly diagnosed cancer and 70% of all cancer deaths (Berger et al., 2006). Additionally, more than 70% of the mortality associated with many cancers, including prostate, bladder, colon, uterus, pancreas, stomach, rectum, and lung occur in patients 65 and older. Men over 75 have the highest rates of cancer at 28 percent. Women 65 and older have rates of 17 percent. Rates for older non-Hispanic Whites are twice as high as for Hispanics and non-Hispanic Blacks. The most common types of cancer found in men are prostate and lung cancer. Breast and lung cancer are the most common forms in women.
In 2008, 27 percent of those 65 and older had diabetes. Diabetes is a problem with your body that causes blood glucose (sugar) levels to rise higher than normal, known as hyperglycemia. Type 2 diabetes is the most common form of diabetes. With type 2 diabetes the body does not use insulin properly (insulin resistance). According to the American Diabetes Association, people with diabetes are 40% more likely to suffer from glaucoma than people without diabetes, and people with diabetes are 60% more likely to develop cataracts. Diabetic retinopathy is a general term for all disorders of the retina caused by diabetes. Nerve damage from diabetes is called diabetic neuropathy, and about half of all people with diabetes have some form of nerve damage (American Diabetes Association, 2018). Rates are higher among Mexican origin individuals and Blacks than non-Hispanic whites. The treatment for diabetes includes dietary changes, increasing physical activity, weight loss for those who are overweight, and medication (National Institute on Aging, 2011).
Shingles: According to the National Institute on Aging (2015e), shingles is a disease that affects your nerves.Shingles is caused by the same virus as chicken pox, the varicella-zoster virus (VZV). After you recover from chickenpox, the virus continues to live in some of your nerve cells. It is usually inactive, and most adults live with VZV in their body and never get shingles. However, the virus will become active in one in three adults. Instead of causing chickenpox again, it produces shingles.A risk factor for shingles includes advanced age as people have a harder time fighting off infections as they get older. About half of all shingles cases are in adults age 60 or older, and the chance of getting shingles becomes much greater by age 70. Other factors that weaken an individual's ability to fight infections, such as cancer, HIV infections, or other medical conditions, can put one at a greater risk for developing shingles.
Shingles results in pain, burning, tingling, or itching in the affected area, as well as a rash and blisters. Typically, shingles develops only on one side of the body or face and in a small area rather than all over. Most cases of shingles last 3 to 5 weeks. After the shingles rash goes away, some people may be left with ongoing pain, called post-herpetic neuralgia (PHN) in the area where the rash had been (NIA, 2015e). The older one is when getting shingles, the greater the chance of developing PHN. Some people with PHN find it hard to go about their daily activities, like dressing, cooking, and eating. They can also suffer from depression, anxiety and sleeplessness. Medicines can help with pain and usually PHN will disappear. Unfortunately, the blisters from shingles may become infected or leave a scar. Blisters near or in the eye can cause lasting eye damage or blindness. There is a shingles vaccine recommended for those aged 60 and older. Shingles is not contagious, but one can catch chickenpox from someone with shingles.
Alzheimer's disease : Probably the most well-known and most common neurocognitive disorder for older individuals is Alzheimer's disease. In 2016 an estimated 5.4 million Americans were diagnosed with Alzheimer's disease (Alzheimer's Association, 2016), which was approximately one in nine aged 65 and over. By 2050 the number of people age 65 and older with Alzheimer's disease is projected to be 13.8 million if there are no medical breakthroughs to prevent or cure the disease (Alzheimer's Assocaiton, 2019). Alzheimer's disease is the 6th leading cause of death in the United States, but the 5th leading cause for those 65 and older. Among the top 10 causes of death in America, Alzheimer's disease is the only one that cannot be prevented, cured, or even slowed. This disease becomes more prevalent with age but is not inevitable. This typically appears after age 60 but develops slowly for years before its appearance. Social support, and aerobic exercise can reduce the risk of Alzheimer's disease. Current estimates indicate that Alzheimer disease affects approximately 50% of those identified with a neurocognitive disorder (Cohen & Eisdorfer, 2011). Alzheimer's disease has a gradual onset with subtle personality changes and memory loss that differs from normal age-related memory problems occurring first. Confusion, difficulty with change, and deterioration in language, problem-solving skills, and personality become evident next. In the later stages, the individual loses physical coordination and is unable to complete everyday tasks, including self-care and personal hygiene (Erber & Szechwan, 2015). Lastly, individuals lose the ability to respond to their environment, to carry on a conversation, and eventually to control movement (Alzheimer's Association, 2016). On average people with Alzheimer's survive eight years, but some may live up to 20 years. The disease course often depends on the individual's age and whether they have other health conditions. The greatest risk factor for Alzheimer's disease is age, but there are genetic and environmental factors that can also contribute. Some forms of Alzheimer's are hereditary, and with the early onset type, several rare genes have been identified that directly cause Alzheimer's. People who inherit these genes tend to develop symptoms in their 30s, 40s, and 50s. Five percent of those identified with Alzheimer's disease are younger than age 65.
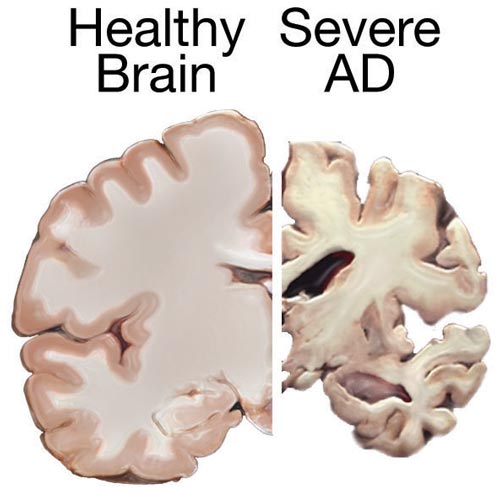
Figure caption: A healthy brain compared to one with sever Alzheimer's Disease. Image courtesy of NIH
According to Erber and Szuchman (2015), the problems that occur with Alzheimer's disease are due to the "death of neurons, the breakdown of connections between them, and the extensive formation of plaques and tau, which interfere with neuron functioning and neuron survival" (p. 50). Plaques are abnormal formations of protein pieces called beta-amyloid. Beta-amyloid comes from a larger protein found in the fatty membrane surrounding nerve cells. Because beta-amyloid is sticky, it builds up into plaques (Alzheimer's Association, 2016). These plaques appear to block cell communication and may also trigger an inflammatory response in the immune system, which leads to further neuronal death.
Where will these people receive care? Seventy percent of AD patients are cared for in the home. Such care can be emotionally, financially, and physically stressful. Most AD patients live 8 to 10 years with the disease and long-term care costs an average of $174,000 per patient (He et al., 2005).
Can you reduce the risk of AD? Yes. Physical and mental inactivity, smoking, obesity, diabetes, hypertension, and depression are all associated with an increased risk for the development of Alzheimer's disease (APA, 1998). Each of these factors can be modified. Keeping mentally and physically active can help preserve cognitive skills, reduce the risk of Alzheimer's disease, and maintain overall health.
Sleep
Similar to other adults, older adults need between 7 to 9 hours of sleep per night, but they tend to go to sleep earlier and get up earlier than those younger. This pattern is called advanced sleep phase syndrome and is based on changes in circadian rhythms (National Sleep Foundation, 2009). There are sleep problems in older adults, and insomnia is the most common problem in those 60 and older (NIA, 2016). People with insomnia have trouble falling asleep and staying asleep . There are many reasons why older people may have insomnia, including certain medications, being in pain, having a medical or psychiatric condition, and even worrying before bedtime about not being able to sleep. Using over the counter sleep aids or medication may only work when used for a short time. Consequently, sleep problems should be discussed with a health care professional.
According to the National Sleep Foundation (2009), there are many medical conditions that affect sleep and include gastroesophageal reflux disease, diabetes mellitus, renal failure, respiratory diseases such as asthma, and immune disorders. Diseases such as Parkinson's disease and multiple sclerosis also commonly cause problems sleeping. Lastly, Alzheimer's disease can interfere with sleeping patterns. Individuals may wake up many times during the night, wander when up, and yell which can alter the amount of time they sleep. Both minor and significant sleep problems in older adults can lead to increased risk of accidents, falls, chronic fatigue, decreased quality of life, cognitive decline, reduced immune function, and depression (Buman, 2013).
Because of sleep problems experienced by those in late adulthood, research has looked into whether exercise can improve their quality of sleep. Results show that 150 minutes per week of exercise can improve sleep quality (Buman, 2013). This amount of exercise is also recommended to improve other health areas including lowering the risk for heart disease, diabetes, and some cancers. Aerobic activity, weight training, and balance programs are all recommended. For those who live in assisted living facilities even light exercise, such as stretching and short walks, can improve sleep. High intensity activity is not necessary to see improvements. Overall, the effects of exercise on sleep may actually be even larger for older adults since their sleep quality may not be ideal to start.
Sexuality
Many older couples find greater satisfaction in their sex life than they did when they were younger. They have fewer distractions, more time and privacy, no worries about getting pregnant, and greater intimacy with a lifelong partner (NIA, 2013). The National Survey of Sexual Health data indicated that 20%-30% of individuals remain sexually active well into their 80s (Schick et al., 2010). However, there are issues that occur in older adults that can adversely affect their enjoyment of healthy sexual relationships. According to the National Institute on Aging (2013), chronic illnesses including arthritis (joint pain), diabetes (erectile dysfunction), heart disease (difficulty achieving orgasm for both sexes), stroke (paralysis), and dementia (inappropriate sexual behavior) can all adversely affect sexual functioning. Hormonal changes, physical disabilities, surgeries, and medicines can also affect a senior's ability to participate in and enjoy sex. How one feels about sex can also affect performance. For example, a woman who is unhappy about her appearance as she ages may think her partner will no longer find her attractive. A focus on youthful physical beauty for women may get in the way of her enjoyment of sex. Likewise, most men have a problem with erectile dysfunction (ED) once in a while, and some may fear that ED will become a more common problem as they age. If there is a decline in sexual activity for a heterosexual couple, it is typically due to a decline in the male's physical health (Erber & Szuchman, 2015).
Overall, the best way to experience a healthy sex life in later life is to keep sexually active while aging. However, the lack of an available partner can affect heterosexual women's participation in a sexual relationship. Beginning at age 40 there are more women than men in the population, and the ratio becomes 2 to 1 at age 85 (Karraker et al., 2011). Because older men tend to pair with younger women when they become widowed or divorced, this also decreases the pool of available men for older women (Erber & Szuchman, 2015). In fact, a change in marital status does not result in a decline in the sexual behavior of men aged 57 to 85 years-old, but it does result in a decline for similar aged women (Karraker et al., 2011).
Theories of Aging (Ob 11, Ob 12)
Why do we age?
There are a number of attempts to explain why we age and many factors that contribute to aging. Genetics, diet, lifestyle, activity, and exposure to pollutants all play a role in the aging process.
Cell Life
Cells divide a limited number of times and then stop. This phenomenon, known as the Hayflick limit. Hayflick limit is evidenced in cells studied in test tubes which divide about 50 times before becoming stopping replication. At the end of each chromosomal strand is a sequence of DNA that does not code for any particular protein, but protects the rest of the chromosome, which is called a telomere. With each replication, the telomere gets shorter. Once it becomes too short the cell does one of three things. It can stop replicating by turning itself off, called cellular senescence. It can stop replicating by dying, called apoptosis. Or, as in the development of cancer, it can continue to divide and become abnormal. Senescent cells can also create problems. While they may be turned off, they are not dead, thus they still interact with other cells in the body and can lead to an increased risk of disease. When we are young, senescent cells may reduce our risk of serious diseases such as cancer, but as we age they increase our risk of such problems (NIA, 2011a). Understanding why cellular senescence changes from being beneficial to being detrimental are still under investigation. The answer may lead to some important clues about the aging process.
Biochemistry and Aging
Free Radical Theory: As we metabolize oxygen, mitochondria ( a cell organelle that uses oxygen to produce energy from food ) in the cells convert oxygen to adenosine triphosphate (ATP) which provides energy to the cell. Unpaired electrons are a byproduct of this process and these unstable electrons cause cellular damage as they find other electrons with which to bond. These free radicals have some benefits and are used by the immune system to destroy bacteria. However, cellular damage accumulates and eventually reduces the functioning of organs and systems. Free radicals are identified with disorders seen in those of advanced age, including cancer, atherosclerosis, cataracts, and neurodegeneration. Many food products and vitamin supplements are promoted as age-reducing. Some research has supported adding antioxidants to our diets to counter the effects of free radical damage because the antioxidants can donate an electron that can neutralize damaged molecules. However, the research on the effectiveness of antioxidants is not conclusive (Harvard School of Public Health, 2016).
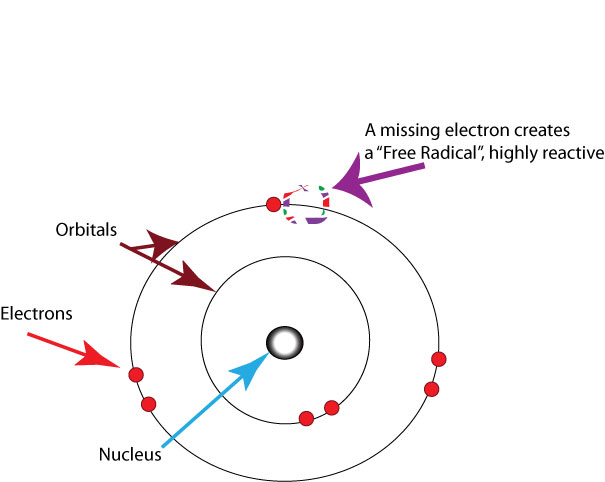
Image courtesy of Healthvalue Wikimedia
Protein Crosslinking: This theory focuses on the role of blood sugar, or glucose, plays in the aging of cells. Glucose molecules attach themselves to proteins and form chains or crosslinks. These crosslinks reduce the flexibility of tissue and tissue become stiff and lose functioning. The circulatory system becomes less efficient as the tissue of the heart, arteries and lungs lose flexibility. And joints grow stiff as glucose combines with collagen. (To conduct your own demonstration of this process, take a piece of meat and place it in a hot skillet. The outer surface of the meat will caramelize and the tissue will become stiff and hard.)
DNA Damage: DNA is part of cells which we discussed the aging process of cells above. Connected to Hayflick's limit, genetic programming theories of aging suggest that the body's DNA genetic code contains a built-in time limit for human cells duplication. These theories promote the view that the cells of the body can only duplicate a certain number of times and that the genetic instructions for running the body can be read only a certain number of times before they become illegible. Further, as we live, DNA is damaged by environmental factors such as toxic agents, pollutants, and sun exposure (Dollemore, 2006). The damage from different environmental factors sometimes cannot be repaired and remains in our DNA. This results in deletions of genetic material, and mutations in the DNA that is duplicated in new cells. The accumulation of these errors results in reduced functioning in cells and tissues.
Decline in the Immune System: As we age, B-lymphocytes and T-lymphocytes become less active. These cells are crucial to our immune system as they secrete antibodies and directly attack infected cells. The thymus, where T-cells are manufactured, shrinks as we age. This reduces our body's ability to fight infection (Berger, 2005). T-cells , or lymphocytes , fight bacteria, viruses, and other foreign threats to the body. T-cells are in a "naïve" state before they are programmed to fight an invader, and become "memory cells". These cells now remember how to fight a certain infection should the body ever come across this invader again. Memory cells can remain in your body for many decades, and why the measles vaccine you received as a child is still protecting you from this virus today. As older adults produce fewer new T-cells to be programmed, they are less able to fight off new threats and new vaccines work less effectively. For example, the reason why the shingles vaccine works well with older adults is because they already have some existing memory cells against the varicella virus. The shingles vaccine is acting as a booster (NIA, 2011a).
Hormonal Stress Theory, also known as Neuroendocrine Theory of Aging, suggests that as we age the ability of the hypothalamus to regulate hormones in the body begins to decline leading to metabolic problems (American Federation of Aging Research (AFAR) 2011). This decline is linked to an excess of the stress hormone cortisol. While many of the body's hormones decrease with age, cortisol does not (NIH, 2014a). The more stress we experience, the more cortisol released, and the more hypothalamic damage that occurs. Changes in hormones have been linked to several metabolic and hormone related problems that increase with age, such as diabetes (AFAR, 2011), thyroid problems (NIH, 2013), osteoporosis, and orthostatic hypotension (NIH, 2014a).
Cognitive Development in Late Adulthood (Ob 13)
There are numerous stereotypes regarding older adults as being forgetful and confused, but what does the research on memory and cognition in late adulthood reveal? Memory comes in many types, such as working, episodic, semantic, implicit, and prospective. There are also many processes involved in memory, thus it should not be a surprise that there are declines in some types of memory and memory processes, while other areas of memory are maintained or even show some improvement with age. In this section, we will focus on changes in memory, attention, problem-solving, intelligence, and wisdom, including the exaggeration of losses stereotyped in the elderly.
The Sensory Register
Aging may create small decrements in the sensitivity of the sensory register. And, to the extent that a person has a more difficult time hearing or seeing, that information will not be stored in memory. This is an important point because many older people assume that if they cannot remember something, it is because their memory is poor. In fact, it may be that the information was never seen or heard.
The Working Memory
Older people have more difficulty using memory strategies to recall details (Berk, 2007). As we age, the working memory loses some of its capacity. A drop in working memory capacity commonly seen in old age. In a study by Göthe, Oberauer, and Kliegl (2007) older and younger adults were asked to learn two tasks simultaneously. Young adults eventually managed to learn and perform each task without any loss in speed and efficiency, although it did take considerable practice. None of the older adults were able to achieve this. Yet, older adults could perform at young adult levels if they had been asked to learn each task individually. Having older adults learn and perform both tasks together was too taxing for the central executive. Older adults get more distracted and use more attention to compensate for their reduced ability to maintain information in working memory. When working memory tasks that do not require much input from the central executive, such as the digit span test, which uses predominantly auditory cues, we find that older adults perform on par with young adults (Dixon & Cohen, 2003). Older adults find it more difficult to concentrate on more than one thing at a time or to keep remember details of an event. However, people compensate for this by writing down information and avoiding situations where there is too much going on at once to focus on a particular cognitive task.
The Long-Term Memory
This type of memory involves the storage of information for long periods of time. Retrieving such information depends on how well it was learned in the first place rather than how long it has been stored. If information is stored effectively, an older person may remember facts, events, names, and other types of information stored in long-term memory throughout life. As you should recall, long-term memory is divided into semantic (knowledge of facts), episodic (events), and implicit (procedural skills, classical conditioning, and priming) memories. Implicit memory requires little conscious effort and often involves skills or more habitual patterns of behavior. This type of memory shows few declines with age. Semantic and episodic memory is part of the explicit memory system, which requires conscious effort to create and retrieve. Several studies consistently reveal that episodic memory shows greater age-related declines than semantic memory (Schwartz, 2011; Spaniol, Madden, & Voss, 2006). It has been suggested that episodic memories may be harder to encode and retrieve because they contain at least two different types of memory, the event, and when and where the event took place. Interestingly, older adults remember more about their early adulthood and adolescence than about middle adulthood (Berk, 2007). Older adults retain semantic memory or the ability to remember vocabulary. Unlike episodic memory, semantic memories are not tied to any particular timeline. Thus, only the knowledge needs to be encoded or retrieved (Schwartz, 2011). Spaniol et al. (2006) found that retrieval of semantic information was considerably faster for both younger and older adults than the retrieval of episodic information, with there being little difference between the two age groups for semantic memory retrieval. They note that older adults' poorer performance on episodic memory appeared to be related to slower processing of the information and the difficulty of the task. They found that as the task became increasingly difficult, the gap between each age groups' performance increased for episodic memory more so than for semantic memory.
Younger adults rely more on mental rehearsal strategies to store and retrieve information. Older adults focus more on external cues such as familiarity and context to recall information (Berk, 2007). And they are more likely to report the main idea of a story rather than all of the details (Jepson & Labouvie-Vief, in Berk, 2007).
A positive attitude about being able to learn and remember plays an important role in memory. When people are under stress (perhaps feeling stressed about memory loss), they have a more difficult time taking in information because they are preoccupied with anxieties. Many of the laboratory memory tests require to compare the performance of older and younger adults on timed memory tests in which older adults do not perform as well. However, a few real-life situations require speedy responses to memory tasks. Older adults rely on more meaningful cues to remember facts and events without any impairment to everyday living.
In general, humans are fairly good at prospective memory if they have little else to do in the meantime. Prospective memories are of events in our future. However, when there are competing tasks that are also demanding our attention, this type of memory rapidly declines. The explanation given for this is that this form of memory draws on the central executive of working memory, and when this component of working memory is absorbed in other tasks, our ability to remember to do something else in the future is more likely to slip out of memory (Schwartz, 2011). However, prospective memories are often divided into time-based prospective memories, such as having to remember to do something at a future time, or event-based prospective memories, such as having to remember to do something when a certain event occurs. When age-related declines are found, they are more likely to be time-based, than event-based, and in laboratory settings rather than in the real world, where older adults can show comparable or slightly better prospective memory performance (Henry, MacLeod, Phillips & Crawford, 2004; Luo & Craik, 2008). This should not be surprising given the tendency of older adults to be more selective in where they place their physical, mental, and social energy. Having to remember a doctor's appointment is of greater concern than remembering to hit the spacebar on a computer every time the word "tiger" is displayed.
Recall versus Recognition: Memory performance often depends on whether older adults are asked to simply recognize previously learned material or recall material on their own. Generally, for all humans, recognition tasks are easier because they require less cognitive energy. Older adults show roughly equivalent memory to young adults when assessed with a recognition task (Rhodes, Castel, & Jacoby, 2008). With recall measures, older adults show memory deficits in comparison to younger adults. While the effect is initially not that large, starting at age 40 adults begin to show declines in recall memory compared to younger adults (Schwartz, 2011).
Attention and Problem-Solving Changes in Attention in Late Adulthood : Changes in sensory functioning and speed of processing information in late adulthood often translates into changes in attention (Jefferies et al., 2015). Research has shown that older adults are less able to selectively focus on information while ignoring distractors (Jefferies et al., 2015; Wascher, Schneider, Hoffman, Beste, & Sänger, 2012), although Jefferies and her colleagues found that when given double time, older adults could perform at young adult levels. Other studies have also found that older adults have greater difficulty shifting their attention between objects or locations (Tales, Muir, Bayer, & Snowden, 2002). Consider the implication of these attentional changes for older adults. How do changes or maintenance of cognitive ability affect older adults' everyday lives? Researchers have studied cognition in the context of several different everyday activities. One example is driving. Although older adults often have more years of driving experience, cognitive declines related to reaction time or attentional processes may pose limitations under certain circumstances (Park & Gutchess, 2000). In contrast, research on interpersonal problem solving suggested that older adults use more effective strategies than younger adults to navigate through social and emotional problems (Blanchard-Fields, 2007). In the context of work, researchers rarely find that older individuals perform poorer on the job (Park & Gutchess, 2000). Similar to everyday problem solving, older workers may develop more efficient strategies and rely on expertise to compensate for cognitive decline. Problem Solving: Problem-solving tasks that require processing non-meaningful information quickly (a kind of task that might be part of a laboratory experiment on mental processes) declines with age. However, many real-life challenges facing older adults do not rely on the speed of processing or making choices on one's own. Older adults resolve everyday problems by relying on input from others, such as family and friends. They are also less likely than younger adults to delay making decisions on important matters, such as medical care (Strough, Hicks, Swenson, Cheng & Barnes, 2003; Meegan & Berg, 2002).
What might explain these deficits as we age? The processing speed theory, proposed by Salthouse (1996, 2004), suggests that as the nervous system slows with advanced age our ability to process information declines. This slowing of processing speed may explain age differences in many different cognitive tasks. For instance, as we age, working memory becomes less efficient (Craik & Bialystok, 2006). Older adults also need a longer time to complete mental tasks or make decisions. Yet, when given sufficient time older adults perform as competently as do young adults (Salthouse, 1996). Thus, when speed is not imperative to the task healthy older adults do not show cognitive declines. In contrast, inhibition theory argues that older adults have difficulty with inhibitory functioning, or the ability to focus on certain information while suppressing attention to less pertinent information tasks (Hasher & Zacks, 1988). Evidence comes from directed forgetting research. In directed forgetting people are asked to forget or ignore some information, but not other information. For example, you might be asked to memorize a list of words, but are then told that the researcher made a mistake and gave you the wrong list, and asks you to "forget" this list. You are then given a second list to memorize. While most people do well at forgetting the first list, older adults are more likely to recall more words from the "forget-to-recall" list than are younger adults (Andrés, Van der Linden, & Parmentier, 2004).
New Research on Aging and Cognition
Can the brain be trained in order to build a cognitive reserve to reduce the effects of normal aging? ACTIVE (Advanced Cognitive Training for Independent and Vital Elderly), a study conducted between 1999 and 2001 in which 2,802 individuals age 65 to 94, suggests that the answer is "yes." These participants (26 percent who were African-American) received 10 group training sessions and 4 follow up sessions to work on tasks of memory, reasoning, and speed of processing. These mental workouts improved cognitive functioning even 5 years later. Many of the participants believed that this improvement could be seen in everyday tasks as well (Tennstedt et al., 2006). Learning new things, engaging in activities that are considered challenging, and being physically active at any age may build a reserve to minimize the effects of primary aging of the brain.
Wisdom
Wisdom is the ability to use common sense and good judgment in making decisions. A wise person is insightful and has knowledge that can be used to overcome obstacles in living. Does aging bring wisdom? While living longer brings experience, it does not always bring wisdom. Paul Baltes and his colleagues (Baltes & Kunzmann, 2004; Baltes & Staudinger, 2000) suggest that wisdom is rare. In addition, the emergence of wisdom can be seen in late adolescence and young adulthood, with there being few gains in wisdom over the course of adulthood (Staudinger & Gluck, 2011). Those who exhibit wisdom may have made wiser choices at younger ages as well. You may have heard that wisdom comes with age. However, wisdom may be more of a function of other factors than cognition. Occupations and experiences that emphasize others rather than self, along with personality characteristics, such as openness to experience and generativity, are more likely to provide the building blocks of wisdom (Baltes & Kunzmann, 2004). Age combined with certain types of experience and/or personality brings wisdom.
Abnormal Loss of Cognitive Functioning During Late Adulthood (Ob 14, Ob 15)
Delirium , also known as acute confusional state, is sudden onset of confusion. Delirium is a decline from a previous level of mental function that develops over a short period of time, typically hours to days. Delirium is a relatively common problem among elderly people while hospitalized (affecting more than 2 million seniors a year), but doctors often dismiss because of the overlapping symptoms are common with dementia, depression, and psychosis. Delirium may manifest from a baseline of existing mental illness, baseline intellectual disability, or dementia, without being due to any of these problems.
Delirium is a syndrome encompassing disturbances in attention, consciousness, and cognition. It may also involve other neurological deficits, such as psychomotor disturbances (e.g. hyperactive, hypoactive, or mixed), impaired sleep-wake cycle, emotional disturbances, and perceptual disturbances (e.g. hallucinations and delusions), although these features are not required for diagnosis. Among older adults, delirium occurs in 15-53% of post-surgical patients, 70-87% of those in the ICU, and up to 60% of those in nursing homes or post-acute care settings. Among those requiring critical care, delirium is a risk for death within the next year.
Historically, the term dementia was used to refer to an individual experiencing difficulty with memory, language, abstract thinking, reasoning, decision making, and problem-solving (Erber & Szuchman (2015). However, in the latest edition of the Diagnostic and Statistical Manual of 381 Mental Disorders Fifth Edition (DSM-5) (American Psychiatric Association, 2013) the term dementia has been replaced by neurocognitive disorder. A Major Neurocognitive Disorder is diagnosed as a significant cognitive decline from a previous level of performance in one or more cognitive domains and interferes with independent functioning, while a Minor Neurocognitive Disorder is diagnosed as a modest cognitive decline from a previous level of performance in one or more cognitive domains and does not interfere with independent functioning. There are several different neurocognitive disorders that are typically demonstrated in late adulthood, and determining the exact type can be difficult because the symptoms may overlap with each other. Diagnosis often includes a medical history, physical exam, laboratory tests, and changes noted in behavior. Neurocognitive disorders can be caused by numerous diseases and circumstances, all of which result in similar general symptoms of impaired judgment, etc. Alzheimer's disease, discussed earlier in the chapter, is the most common neurocognitive disorder, and is incurable. But there are also non-organic causes of dementia that can be prevented. Malnutrition, alcoholism, depression, and mixing medications can result in symptoms of neurocognitive disorders. If these causes are properly identified, they can be treated.
Psychosocial Development in Late Adulthood
Integrity vs. Despair (Ob 16)
How do people cope with old age? Erikson (1980) believed that late adulthood is a time for making sense out of one's life, finding meaning to one's existence, and adjusting to inevitable death. He called this stage integrity vs. despair. This stage includes, "a retrospective accounting of one's life to date; how much one embraces life as having been well lived, as opposed to regretting missed opportunities," (Erikson, 1982, p. 112). Those in late adulthood need to achieve both the acceptance of their life and the inevitability of their death (Barker, 2016). This stage includes finding meaning in one's life and accepting one's accomplishments, but also acknowledging what in life has not gone as hoped. It is also feeling a sense of contentment and accepting others' deficiencies, including those of their parents. This acceptance will lead to integrity, but if elders are unable to achieve this acceptance, they may experience despair. Bitterness and resentments in relationships and life events can lead one to despair at the end of life. According to Erikson (1982), successful completion of this stage leads to wisdom in late life.
Many older adults want to remain active and work toward replacing opportunities lost with new ones. Those who prefer to keep themselves busy demonstrate the Activity Theory , which states that greater satisfaction with one's life occurs with those who remain active (Lemon, Bengston, & Peterson, 1972). Not surprisingly, more positive views on aging and greater health are noted with those who keep active than those who isolate themselves and disengage with others. Community, faith-based, and volunteer organizations can all provide those in late adulthood with opportunities to remain active and maintain social networks. Erikson's concept of generativity applies to many older adults, just as it did in midlife.
Work & Retirement
Older adults are working longer. Jobs that require social skills, accumulated knowledge, and relevant experiences favor older adults (Erber & Szuchman, 2015). Older adults also demonstrate lower rates of absenteeism and greater investment in their work. By 2018, 24 percent of men and about 16 percent of women ages 65 and older were in the labor force. These levels are projected to rise further by 2026, to 26 percent for men and 18 percent for women (U.S. Census Burearu, 2018). Older adults constitute about 5.6% of the U.S. labor force (AOA, 2016). U.S. Census Bureau data (2019) shows that the average retirement age in the United States comes in at about age 65 for men and 63 for women. In the United States, to receive full benefits from Social Security depends on one's age. For those born between 1943 and 1954, they must wait until age 66 for full benefits. It is currently 66 years and two months for those born after 1955 and will gradually increase to 67 for those born after 1960. For those born before 1938, they can receive full social security benefits at age 65. Medicare health insurance is another entitlement that is not available until one is aged 65.
Mandatory retirement is illegal in the United States. In 1986 the Age Discrimination in Employment Act (ADEA) was amended, and mandatory retirement was eliminated for most workers (Erber & Szuchman, 2015). Pilots, air traffic controllers, federal law enforcement, national park rangers, and firefighters continue to have enforced retirement ages. We find that many do choose retirement by age 65 and most leave work by choice. Those who do leave by choice adjust to retirement more easily. Chances are, they have prepared for a smoother transition by gradually giving more attention to an avocation or interest as they approach retirement. And they are more likely to be financially ready to retire. For most Americans, retirement is a process and not a one-time event (Quinn & Cahill, 2016). For those that retire, 60% of workers transition straight to bridge jobs, which are often part-time, and occur between a career and full retirement. About 15% of workers get another job after being fully retired. This may be due to not having adequate finances after retirement or not enjoying their retirement. Approximately 10% of workers begin phasing into retirement by reducing their hours.

Image courtesy of Picpedia
Delayed Retirement: Older adults primarily choose to delay retirement due to economic reasons (Erber & Szchman, 2015). Financially, continuing to work provides not only added income but also does not dip into retirement savings which may not be sufficient. Historically, there have been three parts to retirement income; that is, social security, a pension plan, and individual savings (Quinn & Cahill, 2016). With the 2008 recession, pension plans lost value for most workers. Consequently, many older workers had to work later in life to compensate for absent or minimal pension plans and personal savings. Social security was never intended to replace full income, and the benefits provided may not cover all the expenses, so elders continue to work. Unfortunately, many older individuals are unable to secure later employment, and those especially vulnerable include persons with disabilities, single women, and individuals with intermittent work histories. Some older adults delay retirement for psychological reasons, such as health benefits and social contacts. Recent research indicates that delaying retirement has been associated with helping one live longer. When looking at both healthy and unhealthy retirees, a one-year delay in retiring was associated with a decreased risk of death from all causes (Wu, Odden, Fisher, & Stawski, 2016). When individuals are forced to retire due to health concerns or downsizing, they are more likely to have negative physical and psychological consequences (Erber & Szuchman, 2015). Men, especially, can find unexpected retirement difficult. Women may feel less of an identity loss after retirement because much of their identity may have come from family roles as well. But women tend to have poorer retirement funds accumulated from work and if they take their retirement funds in a lump sum (be that from their own or from a deceased husband's funds), are more at risk of outliving those funds. Women need better financial retirement planning.
Education
Twenty percent of people over 65 have a bachelors or higher degree. And over 7 million people over 65 take adult education courses (U. S. Census Bureau, 2011). Lifelong learning through continuing education programs on college campuses or programs known as "Elderhostels" which allow older adults to travel abroad, live on campus and study provide enriching experiences. Academic courses, as well as practical skills such as computer classes, foreign languages, budgeting, and holistic medicines, are among the courses offered. Older adults who have higher levels of education are more likely to take continuing education. But offering more educational experiences to a diverse group of older adults, including those who are institutionalized in nursing homes can bring enhance the quality of life.
Volunteering: Face-to-face and Virtually
Research suggests that generativity is not just a concern for midlife adults, but for many elders, concerns about future generations continue into late adulthood, and they are volunteering in their community. About 40 percent of older adults are involved in some type of structured, face-to-face, volunteer work. But many older adults, about 60 percent, engage in a sort of informal type of volunteerism helping out neighbors or friends rather than working in an organization (Berger, 2005). They may help a friend by taking them somewhere or shopping for them, etc. Some do participate in organized volunteer programs but interestingly enough, those who do tend to work part-time as well. Those who retire and do not work are less likely to feel that they have a contribution to make. (It's as if when one gets used to staying at home, their confidence to go out into the world diminishes.) And those who have recently retired are more likely to volunteer than those over 75 years of age.
Older adults who volunteer experience more social contact, which has been linked to higher rates of life satisfaction, and lower rates of depression and anxiety (Pilkington, Windsor, & Crisp, 2012). Longitudinal research also finds a strong link between health in later adulthood and volunteering (Kahana, Bhatta, Lovegreen, Kahana, & Midlarsky, 2013). Lee and colleagues found that even among the oldest-old, the death rate of those who volunteer is half that of non-volunteers (Lee, Steinman, & Tan, 2011). However, older adults who volunteer may already be healthier, which is why they can volunteer compared to their less healthy age-mates
New opportunities exist for older adults to serve as a virtual volunteer by dialoguing online with others from around their world and sharing their support, interests, and expertise. According to an article from AARP (American Association of Retired Persons), virtual volunteerism has increased from 3,000 in 1998 to over 40,000 participants in 2005. These volunteer opportunities range from helping teens with their writing to communicating with 'neighbors' in villages of developing countries. Virtual volunteering is available to those who cannot engage in face-to-face interactions and opens up a new world of possibilities and ways to connect, maintain identity, and be productive (Uscher, 2006).
Self-identity and productivity in Old Age (Ob 17)
Older adults continue to want to remain active and work toward replacing opportunities lost with new ones. People in late adulthood continue to be productive in many ways. These include work (even after retirement), education, volunteering, family life, and intimate relationships. Continuity theory suggests that as people age, they continue to view the self in much the same way as they did when they were younger. Their approach to problems, goals, and situations is much the same as it was before. They are the same individuals, but simply in older bodies. Consequently, older adults continue to maintain their identity even as they give up previous roles. For example, a retired Coast Guard commander attends reunions with shipmates, stays interested in new technology for home use, is meticulous in the jobs he does for friends or at church, and displays mementos of life on the ship. He is able to maintain a sense of self as a result. We do not give up who we are as we age. Hopefully, we are able to share these aspects of our identity with others throughout life. Focusing on what a person can do and pursuing those interests and activities is one way to optimize and maintain self-identity.
Political Activism
The elderly are very politically active. Older people are more likely to view voting as a responsibility and to care about a broad range of issues, not just those commonly associated with aging. They are more connected to their communities, which also makes them more likely to vote.They have high rates of voting and engage in letter writing to Congress on issues that not only affect them but on a wide range of domestic and foreign concerns. In the 2008 election, 70 percent of people 65 and older voted. This group tied with 45 to 65-year-olds as having the highest voter turnout (U. S. Census Bureau, 2011). In 2016, this was once again the case, as citizens 65 years and older reported higher turnout (70.9 percent) (U.S. Census Bureau, 2016). In the 2016 presidential election, 71 percent of Americans over 65 voted, compared with 46 percent among 18- to 29-year-olds (U.S. Census Bureau, 2016). Additionally, in the 2018 general election, 58% of poll workers were ages 61 and older, including 27% who were over 70 (Pew Research Center, 2018).
Grandparents raising grandchildren
In chapter 10, middle adulthood, we first discussed grandparting. Older adults continue to be generative and are raising their grandchildren in greater numbers. Grandparenting typically begins in midlife rather than late adulthood, but because people are living longer, they can anticipate being grandparents for longer periods of time. Grandparents may also have the task of raising their grandchildren. According to the 2014 American Community Survey (U.S. Census, 2014a), over 5.5 million children under the age of 18 were living in families headed by a grandparent. This was more than half a million increase from 2010. While most grandparents raising grandchildren are between the ages of 55 and 64, approximately 25% of grandparents raising their grandchildren are 65 and older (Office on Women's Health, 2010a). For many grandparents, parenting a second time can be harder. Older adults have far less energy, and often the reason why they are now acting as parents to their grandchildren is because of traumatic events. A survey by AARP (Goyer, 2010) found that grandparents were raising their grandchildren because the parents had problems with drugs and alcohol, had a mental illness, were incarcerated, had divorced, had a chronic illness, were homeless, had neglected or abused the child, were deployed in the military, or had died. While most grandparents state they gain great joy from raising their grandchildren, they also face greater financial, health, education, and housing challenges that often derail their retirement plans than do grandparents who do not have primary responsibility for raising their grandchildren. An increasing number of grandparents are raising grandchildren today. Issues such as custody, visitation, and continued contact between grandparents and grandchildren after parental divorce are contemporary concerns.
Relationships during Late Adulthood (Ob 19, Ob 20)
Relationship with adult children: Many older adults provide financial assistance and/or housing to adult children. There is more support going from the older parent to the younger adult children than in the other direction (Fingerman & Birditt, 2011). In addition to providing for their own children, many elders are raising their grandchildren. Consistent with socioemotional selectivity theory (SST), older adults seek and are helped by, their adult children providing emotional support (Lang & Schütze, 2002). SST maintains that as time horizons shrink, as they typically do with age, people become increasingly selective, investing greater resources in emotionally meaningful goals and activities. According to the theory, motivational shifts also influence cognitive processing. Aging is associated with a relative preference for positive over negative information. This selective narrowing of social interaction maximizes positive emotional experiences and minimizes emotional risks as individuals become older. They systematically hone their social networks so that available social partners satisfy their emotional needs. The French philosopher Sartre observed that "hell is other people".An adaptive way of maintaining a positive affect might be to reduce contact with those we know may negatively affect us, and avoid those who might. SST shows that increased selectivity in human relationships, rather than abstinence, leads to more positive affect.Lang and Schütze, as part of the Berlin Aging Study (BASE), surveyed adult children (mean age 54) and their aging parents (mean age 84). They found that the older parents of adult children who provided emotional support, such as showing tenderness toward their parent, cheering the parent up when he or she was sad, tended to report greater life satisfaction. In contrast, older adults whose children provided informational support, such as providing advice to the parent, reported less life satisfaction. Lang and Schütze found that older adults wanted their relationship with their children to be more emotionally meaningful. Daughters and adult children who were younger tended to provide such support more than sons and adult children who were older. Lang and Schütze also found that adult children who were more autonomous rather than emotionally dependent on their parents, had more emotionally meaningful relationships with their parents, from both the parents' and adult children's point of view.
Friendships: Friendships are not formed in order to enhance status or careers, and may be based purely on a sense of connection or the enjoyment of being together. Most elderly people have at least one close friend. These friends may provide emotional as well as physical support. Being able to talk with friends and rely on others is very important during this stage of life. Bookwala, Marshall, and Manning (2014) found that the availability of a friend played a significant role in protecting the health from the impact of widowhood. Specifically, those who became widowed and had a friend as a confidante reported significantly lower somatic depressive symptoms, better self-rated health, and fewer sick days in bed than those who reported not having a friend as a confidant. In contrast, having a family member as a confidante did not provide health protection for those recently widowed.
Marriage and Divorce: Fifty-six percent of people over 65 are married. The majority of older men and just over 40 percent of older women are married (He et al., 2005). Seven percent of older men and 9 percent of older women are divorced and about 4 percent of older adults have never married. Many married couples feel their marriage has improved with time and the emotional intensity and level of conflict that might have been experienced earlier, has declined. This is not to say that bad marriages become good ones over the years, but that those marriages that were very conflict-ridden may no longer be together, and that many of the disagreement couples might have had earlier in their marriages may no longer be concerned. Children have grown and the division of labor in the home has probably been established. Men tend to report being satisfied with marriage more than do women. Women are more likely to complain about caring for a spouse who is ill or accommodating a retired husband and planning activities. Older couples continue to engage in sexual activity, but with less focus on intercourse and more on cuddling, caressing, and oral sex (Carroll, 2007).
Divorce after long-term marriage does occur but is not very common. However, with the number of older adults on the rise, the divorce rate is likely to increase. A longer life expectancy and the expectation of happiness cause some older couples to begin a new life after divorce after 65. Consider Betty who divorced after 40 years of marriage. Her marriage had never been ideal but she stuck with it hoping things would improve and because she didn't want to hurt her husband's reputation (he was in a job in which divorce was frowned upon). But she always hoped for more freedom and happiness in life and once her family obligations were no longer as great (the children and grandchildren were on their own), she and her husband divorced. Betty characterized this as an act of love in that both she and her ex-husband were able to pursue their dreams in later life. Older adults who have been divorced since midlife tend to have settled into comfortable lives and, if they have raised children, to be proud of their accomplishments as single parents.
Widowhood: Twenty-nine percent of people over 65 are widowed (U. S. Census Bureau, 2011). The death of a spouse is one of life's most disruptive experiences. It is especially hard for men who lose their wives. Often widowers do not have a network of friends or family members to fall back on and may have difficulty expressing their emotions to facilitate grief. Also, they may have been very dependent on their mates for routine tasks such as cooking, cleaning, etc. In addition, they typically expect to precede their wives in death and by losing a wife, have to adjust to something unexpected. However, if a man can adjust, he will find that he is in great demand, should he decide to remarry.
Widows may have less difficulty because they do have a social network and can take care of their own daily needs. They may have more difficulty financially if their husbands have handled all the finances in the past. They are much less likely to remarry because many do not wish to and because there are fewer men available. At 65, there are 73 men to every 100 women. The sex ratio becomes even further imbalanced at 85 with 48 men to every 100 women (U. S. Census Bureau, 2011).
Loneliness or solitude? Loneliness is a discrepancy between the social contact a person has and the contacts a person wants (Brehm et al., 2002). It can result from social or emotional isolation. Women tend to experience loneliness as a result of social isolation; men from emotional isolation. Loneliness can be accompanied by a lack of self-worth, impatience, desperation, and depression. This can lead to suicide, particularly in older, white, men who have the highest suicide rates of any age group, higher than Blacks, and higher than for females. Rates of suicide continue to climb and peaks in males after age 85 (National Center for Health Statistics, CDC, 2002).
Being alone does not always result in loneliness. For some, it means solitude. Solitude involves gaining self-awareness, taking care of the self, being comfortable alone, and pursuing one's interests (Brehm et al., 2002). Winnie, aged 80, describes her life alone as comfortable and meaningful. "I'm up early to take care of my 3-year-old great-granddaughter who stays with me. We play and have lunch and later her mother comes after her. I love to sing and sing all the time. I sing in the choir. . . I enjoy my mornings at the kitchen table with my coffee. And me and Coco (her dog) enjoy sitting in the sun."
Lesbian, gay, bisexual, transgender (LGBT) and interse Elders
Approximately 3 million older adults in the United States identify as lesbian or gay (Hillman & Hinrichsen, 2014). Lesbian, gay, bisexual, transgender (LGBT) and intersex people are unique from their non-LGBTI counterparts in terms of retirement issues, and these populations often have to take extra steps addressing their employment, health, legal and housing concerns to ensure their needs are met. Throughout the United States, there are 1.5 million adults over the age of 65 who identify as lesbian, gay, or bisexual, and two million people above the age of 50 who identify as such. By 2025 that number is expected to rise to more than 7 million (National Gay and Lesbian Task Force, 2006). Despite the increase in numbers, older lesbian and gay adults are one of the least researched demographic groups, and the research there is portrayed a population faced with discrimination. Ageism, heterocentrism, sexism, and racism can combine cumulatively and impact the older adult beyond the negative impact of each individual form of discrimination (Hillman & Hinrichsen, 2014). David and Knight (2008) found that older gay black men reported higher rates of racism than younger gay black men and higher levels of perceived ageism than older gay white men.
Lesbian and gay older adults who belong to ethnic and cultural minorities, conservative religions, and rural communities may face additional stressors. Lesbian and gay older adults who belong to ethnic and cultural minorities, conservative religions, and rural communities may face additional stressors. According to the Centers for Disease Control and Prevention (2011), compared to heterosexuals, lesbian and gay adults experience both physical and mental health differences. More than 40% of lesbian and gay adults ages 50 and over suffer from at least one chronic illness or disability, and compared to heterosexuals they are more likely to smoke and binge drink (Hillman & Hinrichsen, 2014). When compared to heterosexuals, lesbian and gay elders have less support from others as they are twice as likely to live alone and four times less likely to have adult children (Hillman & Hinrichsen, 2014).

Image courtesy of Flickr
Although lesbian and gay older adults face many challenges, more than 80% indicate that they engage in some form of wellness or spiritual activity (Fredrickson-Goldsen et al., 2011). They also gather social support from friends and "family members by choice" rather than legal or biological relatives (Hillman & Hinrichsen, 2014). This broader social network provides extra support to gay and lesbian elders. There is now a national hotline that provides telephone peer-support and local resources for seniors, the Lesbian, Gay, Bisexual and Transgender (LGBT) National Senior Hotline.
Single, Cohabiting, and Remarried Older Adults (Ob 23)
About 4 percent of adults never marry. Many have long-term relationships, however. The never married tend to be very involved in family and caregiving and do not appear to be particularly unhappy during late adulthood, especially if they have a healthy network of friends. Friendships tend to be an important influence on life satisfaction during late adulthood. Friends may be more influential than family members for many older adults. According to socioemotional selectivity theory , older adults become more selective in their friendships than when they were younger (Carstensen, Fung, & Charles, 2003). The socioemotional selectivity theory states that older individuals perceive time as more limited, and instead prioritize emotion-related goals. Older adults, feeling that they have less time left in life, prefer spending time with close others who provide a sense of emotional meaning. Friendships are not formed in order to enhance status or careers and may be based purely on a sense of connection or the enjoyment of being together. Most elderly people have at least one close friend. These friends may provide emotional as well as physical support. Being able to talk with friends and rely on others is very important during this stage of life. According to socioemotional selectivity theory, older adults show improvements in social functioning and psychological well-being because their acknowledgment of less time creates them to prioritize emotional goals.

Image courtesy of Flickr
About 4 percent of older couples choose cohabitation over marriage (Chevan, 1996). As discussed in our chapter on early adulthood, these couples may prefer cohabitation for financial reasons, may be same-sex couples who cannot legally marry, or couples who do not want to marry because of previous dissatisfaction with marital relationships. There are between 1 and 3 million gay and lesbian older adults in America today and numbers will continue to increase (Cahill et al., 2000). These older adults have concerns over health insurance, being able to share living quarters in nursing homes and assisted living residences where staff members tend not to be accepting of homosexuality and bisexuality. SAGE (Senior Action in a Gay Environment) is an advocacy group working on remedying these concerns. Same-sex couples who have endured prejudice and discrimination through the years and can rely upon one another continue to have support through late adulthood. Those who are institutionalized, however, may find it harder to live together.
Couples, who remarry after midlife, tend to be happier in their marriages than in first marriage. These partners are likely to be more financially independent, have children who are grown, and enjoy greater emotional wisdom that comes with experience.
Older Adults, Caregiving, and Long-Term Care (Ob 21, Ob 22)

Photo Courtesy of Raychan on Unsplash
We previously noted the number of older adults who require long-term care and noted that the number increases with age. Most (70 percent) of older adults who require care receive that care in the home. Most are cared for by their spouse, or by a daughter or daughter-in-law. However, those who are not cared for at home are institutionalized. In 2008, 1.6 million out of the total 38.9 million Americans age 65 and older were nursing home residents (U. S. Census Bureau, 2011). Among 65-74, 11 per 1,000 adults aged 65 and older were in nursing homes. That number increases to 182 per 1,000 after age 85. More residents are women than men, and more are Black than white. As the population of those over 85 continues to increase, more will require nursing home care. Meeting the psychological and social as well as physical needs of nursing home residents is a growing concern. Rather than focusing primarily on food, hygiene, and medication, quality of life within these facilities is important. Residents of nursing homes are sometimes stripped of their identity as their personal possessions and reminders of their lives are taken away. A rigid routine in which the residents have little voice can be alienating to an older adult. Routines that encourage passivity and dependence can be damaging to self-esteem and lead to further deterioration of health. Greater attention needs to be given to promoting successful aging within institutions.
Elderly Abuse (Ob 24)
Current research indicates that at least 1 in 10, or approximately 4.3 million, older Americans are affected by at least one form of elder abuse per year (Roberto, 2016). Those between 60 and 69 years of age are more susceptible than those older. This may be because younger older adults more often live with adult children or a spouse, two groups with the most likely abusers. Perpetrators of elder abuse are typically family members and include spouses/partners and older children (Roberto, 2016). Children who are abusive tend to be dependent on their parents for financial, housing, and emotional support. Substance use, mental illness, and chronic unemployment increase dependency on parents, which can then increase the possibility of elder abuse. Victims are usually very frail and impaired and perpetrators are usually dependent on the victims for support. Prosecuting a family member who has financially abused a parent is very difficult. The victim may be reluctant to press charges and the court dockets are often very full resulting in long waits before a case is heard. Granny dumping or the practice of family members abandoning older family members with severe disabilities in emergency rooms is a growing problem. An estimated 100,000 and 200,000 are dumped each year (Tanne in Berk, 2007).

Image courtesy of Needpix
Nursing homes have been publicized as places where older adults are at risk of abuse. Abuse and neglect of nursing home residents is more often found in facilities that are run down and understaffed. Abuse and neglect occurring in a nursing home is estimated to be 25%-30% (Youdin, 2016). Abuse of nursing home residents is more often found in facilities that are run down and understaffed. Cognitive impairment, including confusion and communication deficits, is the greatest risk factor for elder abuse, while a decline in overall health resulting in a greater dependency on others is another. Having a disability also places an elder at a higher risk for abuse (Youdin, 2016).
Definitions of elder abuse typically recognize five types of abuse, physical, psychological/emotional, sexual, financial/exploitation, and neglect. Consequences of elder abuse are significant and include injuries, new or exacerbated health conditions, hospitalizations, premature institutionalization, and early death (Roberto, 2016). Psychological and emotional abuse is considered the most common form, even though it is underreported and may go unrecognized by the elder. Continual emotional mistreatment is very damaging as it becomes internalized and results in late-life emotional problems and impairment. Financial abuse and exploitation is increasing and costs seniors nearly 3 billion dollars per year (Lichtenberg, 2016). Financial abuse is the second most common form after emotional abuse and affects approximately 5% of elders.
Table. Types of Elder Abuse
| Type | Description |
| Physical Abuse | Physical force resulting in injury, pain, or impairment |
| Sexual Abuse | Nonconsensual sexual contact |
| Psychological and Emotional Abuse | Infliction of distress through verbal or nonverbal acts such as yelling, threatening, or isolating |
| Financial Abuse and Exploitation | Improper use of an elder's finances, property, or assets |
| Neglect and Abandonment | Intentional or unintentional refusal or failure to fulfill caregiving duties to an elder |
Adapted from Roberto (2016)
Successful Aging

Photo courtesy of Pixabay
Although definitions of successful aging are value-laden, Rowe and Kahn (1997) defined three criteria of successful aging that are useful for research and behavioral interventions. They Include: Relative avoidance of disease, disability, and risk factors, like high blood pressure, smoking, or obesity; Maintenance of high physical and cognitive functioning; Active engagement in social and productive activities
For example, research has demonstrated that age-related declines in cognitive functioning across the adult life span may be slowed through physical exercise and lifestyle interventions (Kramer & Erickson, 2007). Another way that older adults can respond to the challenges of aging is through compensation. Specifically, selective optimization with compensation is used when the elder adjusts, as needed, in order to continue living as independently and actively as possible (Baltes & Dickson, 2001). The Baltes' model for successful aging argues that across the lifespan, people face various opportunities or challenges such as, jobs, educational opportunities, and illnesses. According to the SOC model, a person may select particular goals or experiences, or circumstances might impose themselves on them. Either way, the selection process includes shifting or modifying goals based on choice or circumstance in response to those circumstances. The change in direction may occur at the subconscious level. This model emphasizes that setting goals and directing efforts towards a specific purpose is beneficial to healthy aging. Optimization is about making the best use of the resources we have in pursuing goals. Compensation, as its name suggests, is about using alternative strategies in attaining those goals. The SOC model covers a number of functional domains—motivation, emotion, and cognition. We might become more adept at using SOC as time moves on, as we work to compensate and adjust for changing abilities across the lifespan. The processes of selection, optimization, and compensation can be found throughout the lifespan. As we progress in years, we select areas in which we place resources, hoping that this selection will optimize the resources that we have, and compensate for any defects accruing from physiological or cognitive changes. When older adults lose functioning, referred to as loss-based selection, they may first use new resources/technologies or continually practice tasks to maintain their skills. However, when tasks become too difficult, they may compensate by choosing other ways to achieve their goals. For example, a person who can no longer drive needs to find alternative transportation, or a person who is compensating for having less energy learns how to reorganize the daily routine to avoid overexertion.
Conclusion
The period of late adulthood, which starts around age 65, is characterized by great changes and ongoing personal development. Older adults face profound physical, cognitive, and social changes, and many figure out strategies for adjusting to them and successfully cope with old age. Proper diet, exercise, and avoidance of health risks can all lead to overall well-being during old age, and sexuality can continue throughout the lifespan in healthy adults. Thus, many older adults can maintain physical and mental strength until they die, and their social worlds can also remain as vital and active as they want. Cognitively, we find that older people adjust quite well to the challenges of aging by adopting new strategies for solving problems and compensating for loss abilities. Although some intellectual abilities gradually decline throughout adulthood, starting at around the age 25, others stay relatively steady (crystalized intelligence). Many cognitive abilities can be maintained with stimulation, practice, and motivation. Socially, many of older adults become adept at coping with the changes in their lives, such as death of a spouse and retirement from work. The death of a spouse has major psychological, social, and material effects on the surviving widow and makes the formation and continuation of friendships highly important. We will explore more about death and dying in the next chapter.
We have a greater understanding of the needs of older adults and more resources identifying the needs necessary to promote healthy aging in our growing population of older adults. We are coming to recognize the strengths of late adulthood and to move beyond the stereotypes of aging. This new appreciation of the value of older adults promises to lay the groundwork for a new approach to this period of life.
Chapter 11 Key terms
| Optimal aging | Hayflick limit |
| Impaired aging | Free Radical Theory |
| Historic racism | Implicit Memory |
| Healthy Life Expectancy (HLE) | Semantic Memory |
| Primary aging | prospective memory |
| Secondary aging | neurocognitive disorder |
| Elderspeak | Integrity vs. despair |
| Alzheimer's disease | socioemotional selectivity theory |
| Chronic illnesses |
Development Through the Lifespan 6th Edition Chapter 11
Source: https://open.maricopa.edu/psy240mm/chapter/chapter-eleven-late-adulthood/
0 Response to "Development Through the Lifespan 6th Edition Chapter 11"
Post a Comment